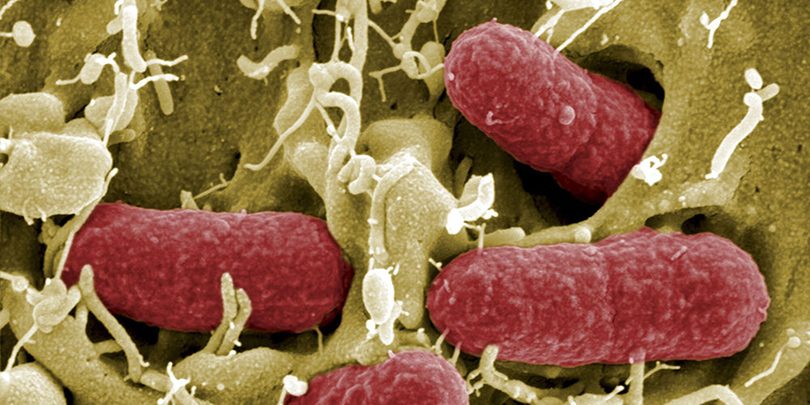
Escherichia coli (E. coli) is a bacteria that establishes itself in the digestive tract of humans and warm-blooded animals. The majority of strains of E. coli are harmless, only a few are pathogenic. This is the case for strains of E. coli so-called enterohemorrhagic (EHEC). The latter cause bloody diarrhea and produce a powerful toxin causing hemolytic uremic syndrome. (SHU). Regularly, strains of ECEH are the cause of food poisoning through the consumption of poorly cooked or raw animal products. Fresh fruits and vegetables, having been in contact with these strains may also be at risk.
SYMPTOMS OF INFECTION
Symptoms caused by ECEH appear between 3 and 8 days after infection. It's abdominal pain and diarrhea, which can evolve into bloody shapes (hemorrhagic colitis). Vomiting and fever may also occur.
At the same time, toxins produced by ECEH (called Shiga-toxins because of their resemblance to those produced by Shigella dysenteriae or Shiga bacillus) destroy the walls of blood vessels and cause clotting problems as well as high blood pressure. At 10% infected people, the spread of Shiga toxins causes a hemolytic uremic syndrome (SHU), deadly in 3 to 5% cases. The latter is characterized by impairment of kidney function and a drop in the concentration of blood cells. (red blood cells and platelets). A quarter of people suffering from HUS also develop neurological complications which can lead to a state of coma.
EPIDEMIOLOGY
ECEH can be the cause of food poisoning (TIA) graves. The first epidemiological data date back to 1982, date the first strain of ECEH was isolated during an outbreak of TIA in the United States. The outbreak was caused by hamburgers with undercooked burgers.. Since, ECEH have caused numerous other epidemic outbreaks and therefore represent a public health problem. One of the serotypes most frequently responsible for these infections is O157.:H7.
In 1996, Japan experienced a major outbreak of TIA caused by serotype O157:H7. Following the consumption of sprouted radish seeds, 9578 cases have been recorded. In 2011, a strain of ECEH belonging to serotype O104:H4 caused a comparable episode in Europe. At the end of the epidemic, whose original home was Germany, European health authorities reported several thousand people poisoned and 47 death. after investigation, sprouted fenugreek seeds imported from Egypt were named as the source of the epidemic.
The incidence of ECEH infections varies according to age groups. It peaks in children younger than 3 years. However, in the case of the European epidemic which occurred in 2011, 7 people on 10 affected were adult females. This unusual distribution of cases among the population can largely be explained by differences in dietary habits. : women, greater consumers of raw vegetables than men, were more affected by the epidemic.
In France, the largest outbreak linked to contaminated frozen hamburgers dates back to 2005. The health authorities had recorded 69 cas, whose 57 concerned children aged less than 13 years.
TRANSMISSION
The transmission of ECEH type pathogens mainly occurs during consumption of contaminated food. The products concerned are generally raw or undercooked meat, raw milk dairy products, and more rarely raw plant products. The natural reservoir of ECEH being mainly the digestive tract of cattle, contamination can also occur during the milking or slaughter of these animals. The feces ruminants present in the soil, in manure and water (mares, streams) are also a possible source of contamination.
Human-to-human transmission of ECEH is also possible, but it occurs more rarely. according to statistics from the National Institute for Health Surveillance, it takes place from child to adult, for example when washing a baby.
TREATMENT
Most antibiotics are not recommended for treating infections at ECEH. By destroying bacteria, these cause the release of Shiga toxins in the body, what can make HUS worse. To avoid this situation, the preferred therapeutic strategy consists of fill the deficiencies caused by Shiga toxins (drop in red blood cells, platelets, kidney damage) par transfusion, dialysis, and plasma exchanges.
Diarrheal episodes are, as for them, treated symptomatically : patients are rehydrated, but do not take anti-diarrheal medications, to allow the elimination of the bacteria and its toxins in the stools.
PREVENTION AND RECOMMENDATIONS
Current knowledge does not make it possible to reduce the incidence of ECEH in cattle populations.. On the other hand, via des tests, it is possible to determine if an animal carries the bacteria. If applicable, the meat can be subjected to bactericidal treatment which consists of heating or irradiating it. These techniques, although effective, do not systematically guarantee the absence of ECEH in foods. To effectively protect against ECEH infections, we must respect theapplication of strict hygiene practices throughout the food chain, from producer to consumer.
Personnel involved in the production and preparation of raw plant and animal products must be trained in good hygiene practices.
Concerning consumers and cooks, Most EHEC infections can be avoided by following the following recommendations: :
– cook ground beef thoroughly, particularly in children under 5 years ;
– young children and the elderly should avoid consuming raw milk cheeses ;
– wash the fruit, vegetables and aromatic herbs, especially if they are eaten raw ;
– wash your hands before preparing meals and as often as necessary ;
– ensure the hygiene of kitchen equipment, especially when it has been in contact with raw meat, to avoid cross contamination ;
– separate cooked foods from raw foods ;
– avoid contact with very young children (less than 5 years) with farm animals, especially cattle, sheep and their environment ;
– do not drink water that is not microbiologically controlled (well, source).
Source : Pastor Institute